What is the gut microbiome?
How is a healthy gut microbiome formed?
Are there cultural differences in what constitutes a health gut microbiome?
Why is a healthy gut microbiome so important for health and longevity?
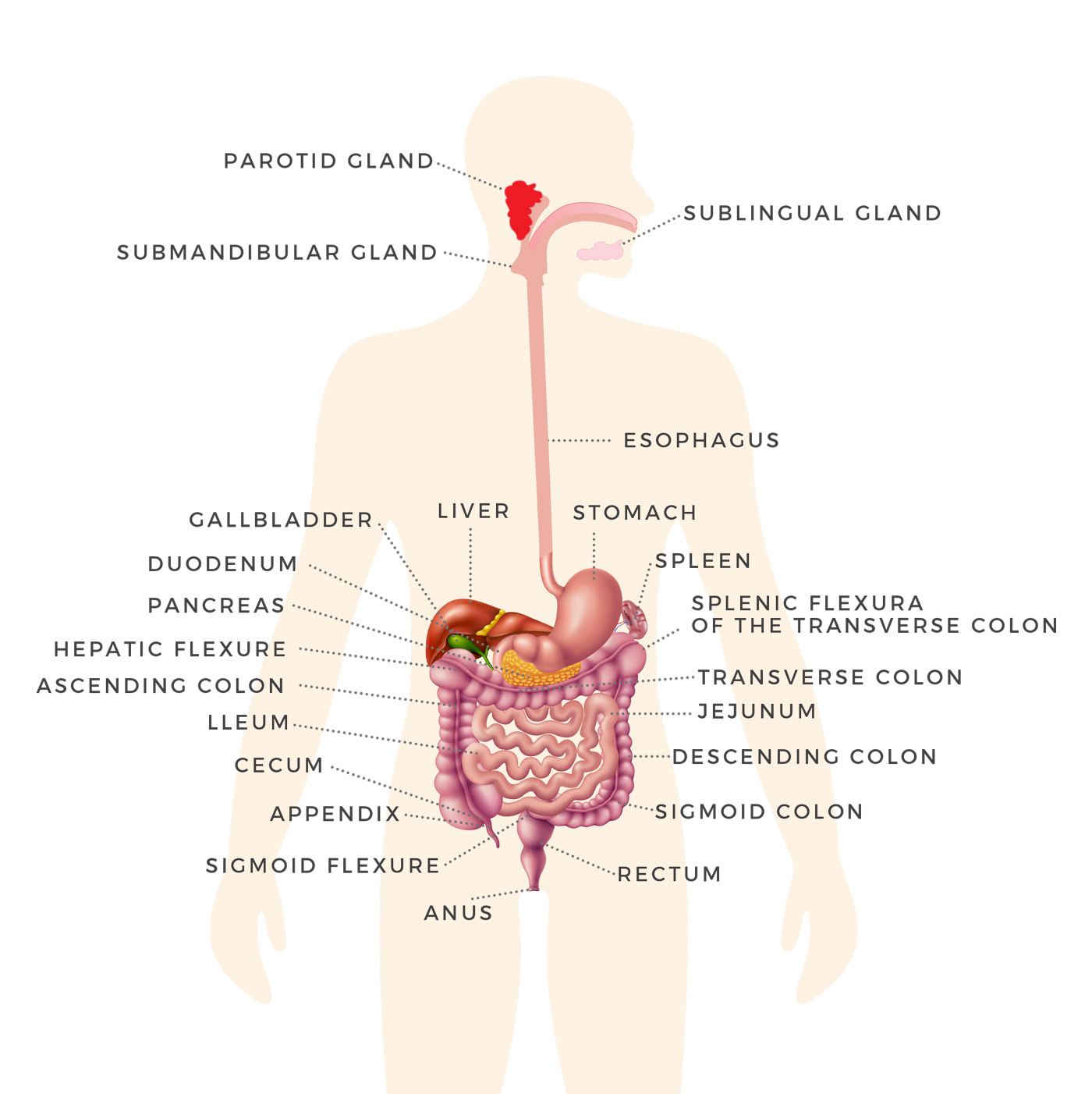
Your ‘gut microbiome’ is made up of the trillions of microorganisms and their genetic material that live in your intestinal tract. The term ‘Microbiota’ refers to the entire population of micro-organisms that colonizes a particular location; and includes not just bacteria, but also other microbes such as fungi, archaea, viruses and protozoans.1
The relationship between the gut microbiota and human health is being increasingly recognized. It is now well-established that a healthy gut flora is largely responsible for the overall health and vitality of the individual.
Although the gut microbiota in an infant appears more haphazard, it starts to resemble the adult flora by three years old.2
With that said, even in adults, there exist both temporal and spatial variations in the microbial distribution from the esophagus to the rectum throughout an individual’s lifespan. In other words, the quantity and type of bacteria is not uniform throughout the entire length of the gastro-intestinal system.
There is strong evidence to demonstrate that there are pronounced differences in the make-up of the gut microbiota of healthy populations when comparing humans from different geographic locations. These distinctive features are evident in early infancy as well as adulthood.3

The normal gut microbiota plays a specific role within the body and is involved in nutrient metabolism, xenobiotic and drug metabolism, maintenance of structural integrity of the gut mucosal barrier, modulation of the immune system, and protection against pathogens.2
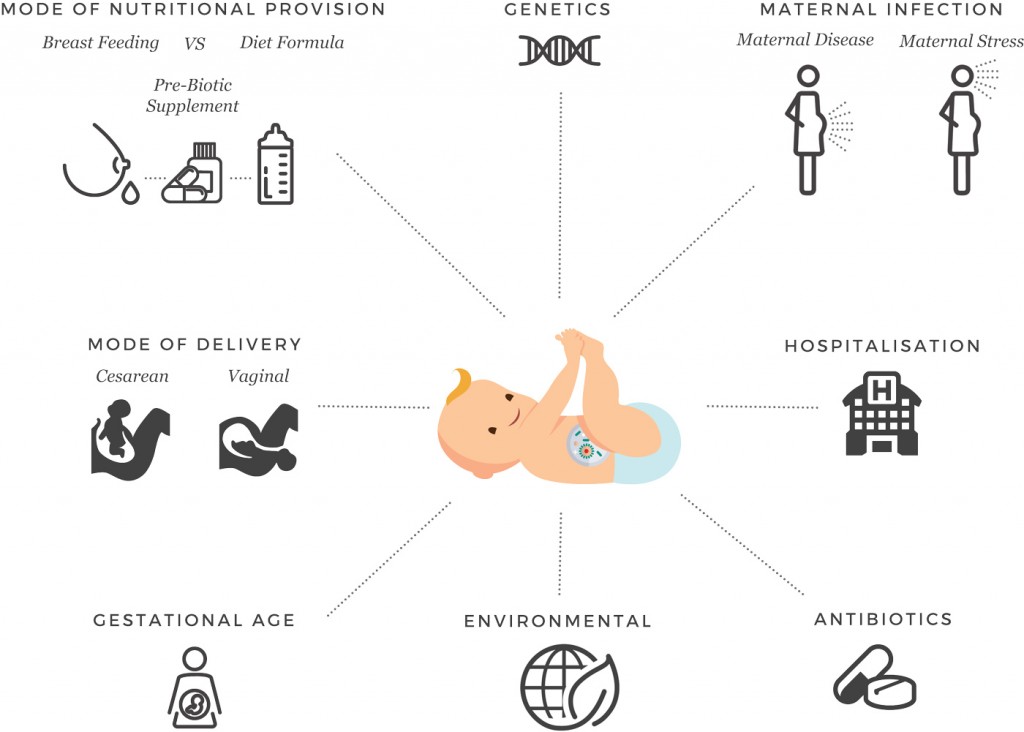
Several factors play a role in shaping the normal gut microbiota. These include:
- The geographic location in which the mother and father were born
- The geographic location in which the mother and father reside
- The geographic location in which the infant is born and resides
- The genetics of the mother and father
- The overall health and vitality of the mother and father at the time of conception
- The overall health and vitality of the mother during pregnancy (Some research suggests a healthy gut microbiome begins in the womb)
- The mode of delivery during birth (vaginal versus caesarean)
- Age
- Diet during infancy (breast milk versus formula feeding)
- Diet during adolescence and adulthood (food quality, vegan-based or meat-based)
- The environment
- Use of antibiotics or antibiotic-like molecules
So, what is a healthy gut?
‘Gut health’ is a term that is increasingly used both within the medical literature and within the health and wellness industry. It covers a multitude of positive aspects of the gastrointestinal (GI) system such as:
- The effective digestion and absorption of food
- The absence of gastrointestinal illness
- Normal intestinal microbiota
- Effective immune status
- And an overall state of wellbeing
Certainly, there is significant evidence to support the notion that the function of the gut extends well beyond food processing and subsequent nutrient and fluid update.
There is ample evidence that two functional entities are key to achieving and maintaining normal gut health: These are the GI microbiome and the GI barrier.7
From a more scientific point view however, it’s still unclear exactly what ‘normal’ gut health is, how it can be accurately defined, and how it can be measured.4 Certainly the gastrointestinal (GI) barrier adjacent to the GI microbiota appears to be a key factor to understanding the complex mechanisms that maintain gut health. Any impairment of the GI barrier can certainly increase the risk of developing infectious, inflammatory, and functional GI diseases, as well as diseases outside the GI system such as autoimmune conditions and metabolic disorders.5, 6
For an in-depth look at the anatomy and physiology of the GI barrier and the problems that can occur (leaky gut), refer back to Part 2 of this blog series on ‘The Human Gut’.
Advancements in technology and testing have allowed scientists to study these microorganisms (the gut microbiota), their function, and key relationships more extensively and to interpret the interactions between microbes and their host in an elaborate manner, both in health and disease.
What factors can have a negative influence on your gut microbiome?
Can certain elements of your lifestyle have a detrimental impact on your gut?
What foods may disrupt the proper functioning of the gut microbiome?
As you are reading this blog, you may be wondering what you can do to prevent yourself from developing an unhealthy gut. And the answer is … ‘plenty’. With that said, there a range of factors that are simply out of your control.
Factors that were predetermined for you and that may predispose you to gut-related issues.
- The genetics of your mother and father
- The overall health and vitality of your mother and father at the time of conception
- The overall health and vitality of your mother during pregnancy
- The mode of delivery during birth (vaginal versus caesarean)
- Your Genetics
- Exposure to antibiotics while in utero or as an infant
- Diet during infancy (breast milk versus formula feeding)
Health and vitality of mother/father
There has been considerable discussion in recent decades around the influence that genetics may have on the ‘health-span’ of an individual. There has been significantly less focus on the relative health and vitality of the mother and father at the time of conception and the role this may play in ‘pre-determining’ the overall health of the baby as it moves through to adolescence and adulthood.
More widely accepted is the notion that female health at the time of conception can influence the quality of the fertilized egg and directly impact on the developing foetus. However, there is also growing evidence that paternal diet, physiology, and environmental factors can impact on sperm quality, post-fertilization development, and adult offspring health.8, 9
New evidence suggests that there is a crucial window of time prior to conception that is important for the lifelong health of the child. Health experts do not agree on the length of time required (ranging from 3 months to 12 months pre-conception), but do agree that a pre-conception ‘clean-up’ of your health should be included in good maternal health.
Health and vitality of mother during pregnancy
The concept of ‘eating for two’ has contributed to a cultural misconception that not only is significantly more food required by the mother during pregnancy, but also that repeated ‘indiscretions’ in food choices are acceptable. However, evidence shows that ill-health or disease during pregnancy can have a lifelong impact on the baby.
Some evidence suggests that a healthy microbiome begins in the womb.
For example, exposure in utero to maternal diabetes carries several short-term consequences for the developing foetus. Current evidence also supports the concept that adult health and disease have developmental origins, and that disorders experienced while the foetus is within the womb can prompt ‘imprinting’ that results in a greater risk of negative health outcomes later in life. In particular, exposure to maternal diabetes seems to influence long-term health, carrying a higher risk of obesity and type 2 diabetes.10 This may then create a vicious cycle for future generations.
The mode of delivery during birth (vaginal versus caesarean)
Since 1985, the World Health Organization has long recommended that the ideal C-section rate should be between 10-15%. Since then, caesarean sections have become increasing common in both developed and developing countries. With Australia’s C-section rate climbing to above 30% of all births, the question is whether this may be having a detrimental impact on the lifelong health of our newly born infants.12
The infant’s intestinal microbiota are believed to be transmitted from the mother to the baby at birth, as the baby exits through the vaginal canal.13, 14 This transmission of bacteria is even suggested to represent a form of epigenetic inheritance.15 What has been shown is that the infant’s immune system develops in tight interaction with the intestinal microbiome, which guides the maturation of the baby and may significantly influence the risk of immune-related diseases.16
So, the question is whether the increased rate of caesarean section births may negatively influence the lifelong health of the baby? And certainly there is a growing body of evidence to suggest that it may negatively impact on the child’s cognitive development, while increasing their risk for type 1 diabetes, asthma and obesity.17, 18
Further evidence is required to determine the role that altered gut microbiota may be playing in the increased of these diseases and developmental challenges faced by C-section babies.
Your Genetics
Recent scientific studies have revealed that variations in many human genes involved in immunity and gut architecture are associated with an altered composition of the gut microbiome.52, 53
Although many factors have the potential to affect the microbial organisms within the gut, a number of recent findings support the hypothesis that certain genetic variations may predispose an individual towards microbiome dysbiosis.54, 55, 56
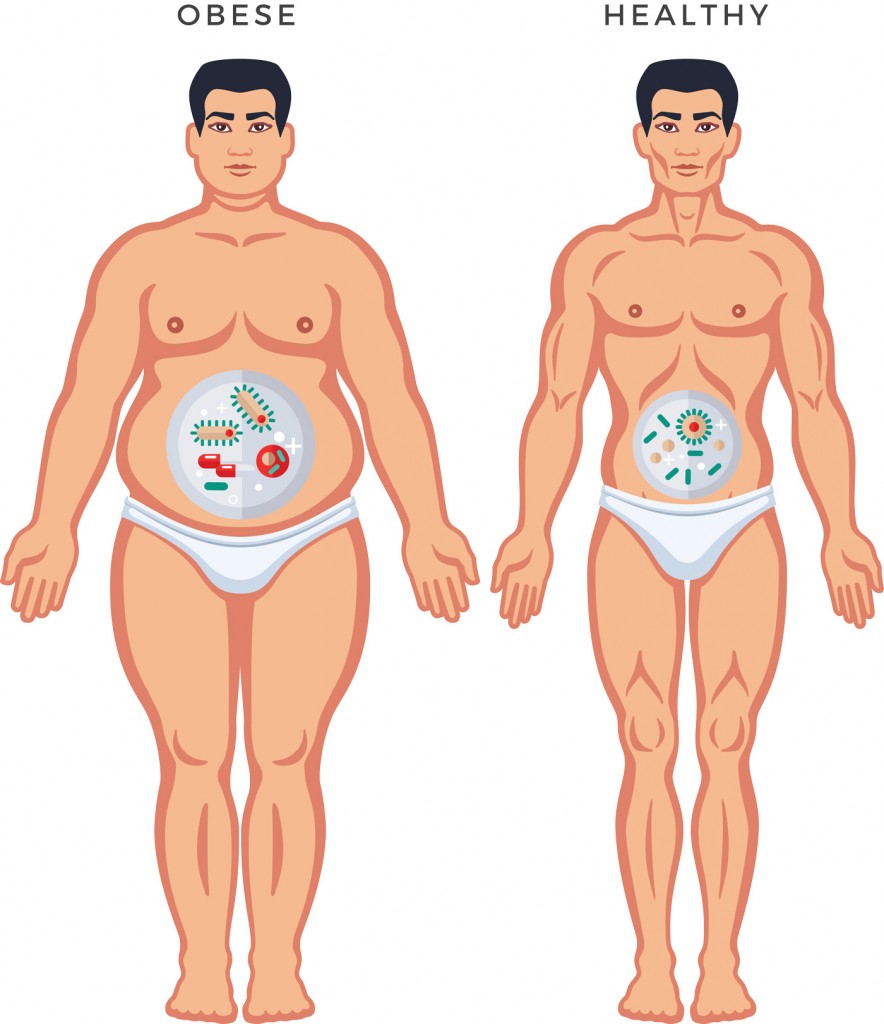
Obesity has been shown to be associated with alterations in the abundance of specific microbial species (some species being under-represented while other are over-represented). Several of these species have been shown to have the capability of being inherited, strengthening the genetic link to obesity.53, 57
Exposure to antibiotics while in utero or immediately following birth
Numerous studies have demonstrated that intrapartum antibiotics are associated with infant gut microbiota dysbiosis, including alterations in overall microbiota community structure, reductions in microbiota richness and a depletion of specific strands of bacteria.19 These changes persisted at 3 months of age. Interesting to note that some of these changes were mitigated in infants who were breastfed exclusively.
Diet during infancy (breast milk versus formula feeding)
There is a wide body of evidence to demonstrate that breastfeeding is nutritionally, immunologically, neurologically, endocrinologically, economically, and ecologically superior to breastmilk substitutes such as formula.20, 21 And it has been shown that infants, children, and mothers who do not breastfeed experience an increased risk of mortality and morbidity.20
The proposed mechanisms behind these increased risks of not breastfeeding includes alternations to the gut microbiota. A wide-ranging set of scientific data demonstrates that positive effects that breastfeeding has on the development of a healthy gut flora in the infant.19, 22, 23
Study finds that 30 percent of the beneficial bacteria in a baby’s intestinal tract come directly from mother’s milk, and an additional 10 percent comes from skin on the mother’s breast.22
By being aware of the contributing factors listed above, you can now see how you can have a positive impact on the health and vitality of generations to come. Either by adhering to these ‘foundation principles’ of human health yourself and within your family, or by educating others as to their importance.
Diet, Lifestyle, Environment
There is growing recognition of the role of diet, lifestyle and other environmental factors in modulating the composition and metabolic activity of the human gut microbiota, which in turn can impact overall health.
- Diet during adolescence and adulthood
- Lifestyle
- Medications
- The environment
- Chemicals
- Antibiotics
Diet during adolescence and adulthood (food quality, vegan-based or meat-based)
Of all the exogenous factors affecting the gut microbiome, a long-term diet appears to have the largest effect to date. Recent research on the effects of dietary interventions has shown that the gut microbiome and its activity can change dramatically with diet.24, 25, 28
The traditional ‘Western Diet’ is laden with processed foods, higher intake of animal-derived foods, commercially raised meats, seafood and eggs, while containing sweets, desserts, and highly processed carbohydrates such as breads, cereals, and pasta. By default, it is lower in whole foods such as fruits, vegetables, whole grains, and herbs. Furthermore, little attention is paid to location in which the food is produced or respect of the seasonal availability and biodiversity of the food.
The standard ‘Western Diet’, which is full of processed foods, also exposes the human gut to a wide range of harmful food additives. One of the most widely studied group of food additives is emulsifiers which are added to most processed foods to aid texture and extend shelf-life. There are numerous studies demonstrating the harmful effects of emulsifiers and their role in contributing to gut dysbiosis.29, 30 One has to question what effect the hundreds of other food additives are having on the proper functioning of the gut.
In contrast, the Mediterranean dietary patterns are characterized by the consumption of whole foods, whole grains, legumes, nuts, vegetables and fruits, consumed in high amounts and frequently. These types of diets also include a reduction in the consumption of fish or seafood, white meat and eggs, moderate to small amounts of poultry and dairy products and minimal consumption of alcohol. The primary source of dietary fats come from olive oil. Water consumption is typically high as well.26
Of course, it wouldn’t surprise you to find out that the Mediterranean-like diets have been associated with a lower incidence of disease and all-cause mortality.26
Although further research is required to isolate the exact mechanisms, it’s logical to think that a whole-food diet, similar to a Mediterranean diet, would preserve microbiota homeostasis and as such have positive immune-regulating benefits.
“Diet-induced changes to gut-associated microbial communities are now suspected of contributing to the growing epidemic of chronic illness in the developed world, including obesity and inflammatory bowel disease.” 27
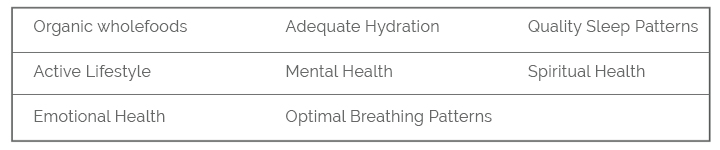
Lifestyle
A significant amount of research is being done to better understand how changes to the gut microbiome can impact on disease. Epigenetic changes are thought to occur in response to a wide variety of factors including body fat percentage, physical activity, nutrition, quality of the water ingested, environmental factors, smoking, alcohol consumption, and psycho-emotional stress.
Epigenetics, as a simplified definition, is the study of biological mechanisms that will switch genes on or off.
Studies have shown that arsenic, chlorine, and cadmium in drinking water can alter the composition of the gut microbiome.31 Likewise, there is evidence to support they hypothesis that chronic psycho-emotional stress can negatively impact on the gut microbiome and directly influence the gut-brain axis.32
So, it would appear that the adherence to the ‘Foundation Principles of Health’ is essential for maintaining a healthy gut microbiome.
Medications/Antibiotics
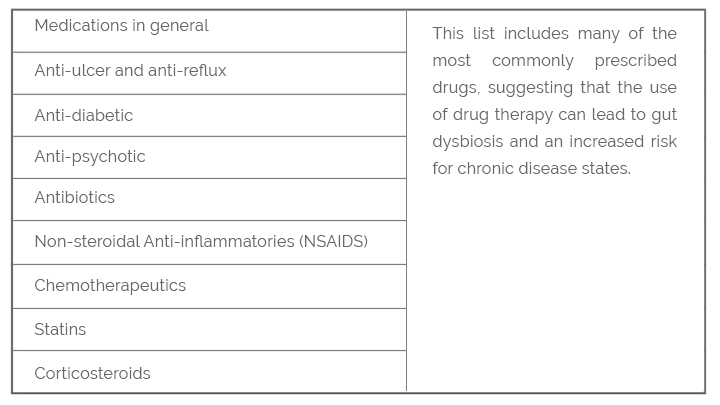
In recent years, there has been accumulating evidence for a strong impact of prescription medications on the gut microbiota composition.
The growing body of evidence implicates the following classes of drugs:
The Environment/Chemicals
Exposure to chemicals within our environment can come from a very wide range of potential sources.

Glyphosate is the active ingredient in the most widely used herbicide in the world, Monsanto’s Roundup.37 Traces of this chemical have been found in sugar, corn, soy, and wheat. Repeated exposure to this chemical has been linked to diabetes, obesity, depression, autism, Alzheimer’s disease, cancer and cardiovascular disease.38
Beyond just the chemicals used to grow commercially grown foods, added food chemicals can be equally harmful to the gut microbiome and our health. This includes food additives such as potassium bromate, emulsifiers, artificial sweeteners, and antibiotics and hormones found in animal products.
The emerging view on environmental toxins is that the impact on our overall health can be devastating.A detailed discussion on this topic is outside the scope of this article, but common environmental toxins include BPA, chlordane, DDE, dioxin, HCB, PCBs, PDBEs, phthalates, tributyitin, triclosan and heavy metals.31
Now that we understand the importance of a healthy gut microbiome and the factors that can negatively affect its make-up and proper functioning, a natural progression would be to consider the potential risks of gut dysbiosis and the correlation to ill-health and disease within the body.
Now that we understand the importance of a healthy gut microbiome and the factors that can negatively affect its make-up and proper functioning, a natural progression would be to consider the potential risks of gut dysbiosis and the correlation to ill-health and disease within the body.
What are the potential consequences of having an unhealthy gut microbiome?
What diseases and medical conditions are linked to gut dysbiosis?
Dysbiosis, which can be described as an imbalance of the flora in the gut microbiome, has been associated with a wide range of medical conditions including:
- Allergies
- Alzheimer’s dementia
- Anxiety
- Asthma
- Atopic dermatitis
- Autism
- Autoimmune conditions
- Cancer (colorectal, breast, ovarian, endometrial)
- Celiac Disease
- Chronic fatigue syndrome
- Cognitive development, brain disorders
- Colon polyps
- Coronary artery disease (CAD)
- Depression
- Diabetes
- Eczema
- Inflammatory bowel disease (ulcerative colitis, Crohn’s disease)
- Irritable bowel syndrome (IBS)
- Metabolic syndrome
- Multiple sclerosis
- Neurodevelopmental illness, neurodegenerative diseases
- Obesity
- Pancreatic disease
- Parkinson’s disease
- Small intestinal bacterial overgrowth (SIBO)
- Skin disorders such as eczema, psoriasis, rosacea
- Systemic inflammation
- Thyroid disease
- Vitiligo
Source: 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51
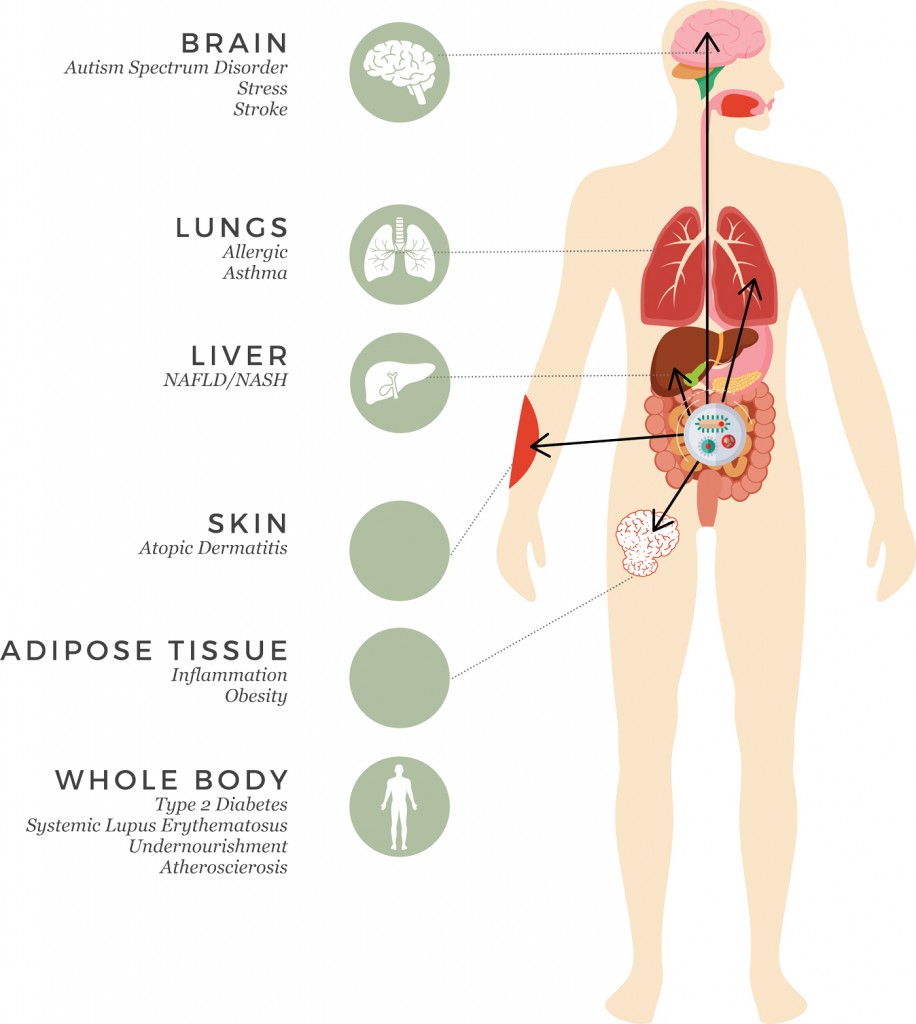
As we contemplate the long list of diseases listed above, we can reflect on the relative importance of the gut microbiome. And in doing so, appreciate that the gut microbiome is much like its own immune system – a collection of cells that work in unison with the human body and that can promote health but sometimes initiate disease.
Knowledge of the factors that affect the gut microbiome is of great importance because dysbiosis of the gut microbiome has been implicated in so many diseases. And with this knowledge, the skilled practitioner may recognize the possibility of a new route for therapeutic intervention.
What tests are available to determine the health of your gut microbiome?
How can you determine if any unhealthy gut microbiome is contributing to your symptoms, disease process or medical condition?
At this point you may be wondering whether gut dysbiosis is contributing to your unwanted symptoms or underlying disease. You may also be questioning how you can get your gut health tested.
And certainly these are great questions.
Gut ‘cleanses’ have become a hot topic world-wide in recent years, with new diets and new products appearing on the market on an almost weekly basis. More and more people are now open to trying out a cleanse, ‘playing around’ with their lifestyle habits, or increasing their intake of fermented veggies or bone broth to see how they feel. But rarely, are we given a precise view into what’s actually going on within our own gut microbiome, despite it being an immensely important component of overall health and vitality.
We are living in exciting times with amazing advancements in overall gut health diagnostic testing. And functional medicine is on the cutting edge of making these lab tests available to patients. These tests can provide valuable insight into why common gastrointestinal problems like acid reflux, constipation, diarrhoea, bloating and IBS are going on in the first place.
Moreover, you don’t necessarily have to be suffering gut symptoms to have underlying gut problems. Many people don’t experience any gut issues at all but are seeing the ripple effects of gut microbiome issues (dysbiosis) in the form of hormonal, skin, cognitive or immunological issues.
It’s important to note that not everyone will require gut health diagnostic testing. A comprehensive health history by a skilled functional medicine practitioner can help you determine whether it is relevant for you.
Comprehensive Stool Testing
This lab test shows the overall ‘landscape’ of your gut microbiome. Basically, the more diverse your gut bacteria, the greater your overall health. In people with health problems, the practitioner can see lower levels or missing colonies of healthy bacteria.
In addition to looking at the variety of bacteria within your gut, this lab also allows your practitioner to look for any unwanted ‘bugs’ that may be overgrowing – namely bacterial, yeast, and parasitic overgrowths. We all have some opportunistic yeast in our guts, but like everything, if it’s out of balance then problems can occur.
‘Who’s running this show anyway!’
This lab test also measures gut inflammation levels, digestion and absorption rates, immune function, and short chain fatty acids.
In most cases, a three-day stool collection is recommended to get a more accurate reflection of what your gut microbiome really looks like. The comprehensive stool sample is often paired with other tests such as SIBO breath test, or intestinal permeability test.
How can you restore the health of your gut microbiome?
What role do healthy foods play in healing your gut?
What role do supplements play in the restoration of a healthy gut?
If you’re suffering from ill-health or disease, the first step should be to consult with a skilled integrative health practitioner who has strong skills in advanced diagnostic testing. Although hard to find, this type of functional medicine practitioner is worth their weight in gold. Not only will this save you a significant amount of time and money, it will also give you the greatest chance of finding out what is truly going on in your body and whether dysbiosis may be playing a significant role in this process.
There is no question that one of the most profound impacts you can have on your health or any disease process is to begin adhering to the ‘Foundation Principles’ of health.
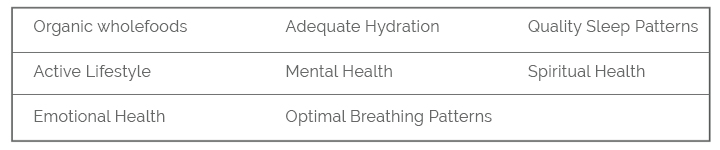
These ‘pillars’ of health are the support your body needs to overcome ill-health and disease.
- Shower and bath in filtered water
- Drink and cook with filtered water
- Maintain healthy sleeping patterns
- Adhere to a strict whole-food diet, free from additives, preservatives, hormones and antibiotics.
- Eliminate exposure to chemicals and other toxins in your personal care products, home cleaning products, home and work environment
- Maintain an active lifestyle with an exercise intensity that is appropriate to your level of health and vitality
- Practice mindfulness daily with a focus on mental, emotional and spiritual health.
Healing from any disease is unique to the individual, and healing from dysbiosis is no different. It requires appropriate testing to be performed up front to identify the extent to which your gut is inflamed and interpret the overall ‘landscape’ of your gut microbiome.
Only through accurate testing and systematic analysis can a structured plan for healing be put in place. With that said, there are commonalities that exist in the healing pathway for most patients.
- Remove foods that are causing inflammation within the gut
- Replace the essential nutrients
- Repair the damage that has been done (In some instances where bacterial, yeast or parasitic overgrowth is present, a therapeutic cleanse is required to regain balance)
- Reinoculate the good bacteria and regain a healthy gut microbiome
At Effortless Superhuman, our holistic healing practitioners use world-class, medical grade supplementation for all treatment protocols. This quality leads to a fast-tracking of the healing process and helps them to achieve superior results.
