 Vertigo is more than just a fleeting sensation of dizziness — for many individuals, it can be a disorienting and debilitating condition that significantly affects daily life. At our holistic physiotherapy clinic in West Perth, we understand that vertigo is not just a symptom but a signal that something deeper is occurring within the vestibular system. Our integrated approach combines evidence-based physiotherapy techniques with a personalised, whole-body focus to help restore balance and confidence in our patients.
Vertigo is more than just a fleeting sensation of dizziness — for many individuals, it can be a disorienting and debilitating condition that significantly affects daily life. At our holistic physiotherapy clinic in West Perth, we understand that vertigo is not just a symptom but a signal that something deeper is occurring within the vestibular system. Our integrated approach combines evidence-based physiotherapy techniques with a personalised, whole-body focus to help restore balance and confidence in our patients.
What is Vertigo and How Common is It?
Vertigo is defined as the sensation of movement or spinning when one is actually stationary. Unlike general dizziness, which may include lightheadedness or feeling faint, vertigo is characterized by the illusion of motion — either the person feels they are moving, or that their environment is.
It’s a relatively common condition. According to the Australian Institute of Health and Welfare, approximately 2-3% of the population will experience significant vertigo at some point in their lives. It is particularly prevalent among older adults but can affect individuals of all ages.
What Are the Main Causes of Vertigo?
Vertigo arises from dysfunction in the vestibular system, which includes the inner ear, brainstem, and associated neural pathways that control balance and spatial orientation. The most common causes include:
| Brain Hemispheres | Vagal Nerve | PMRF |
| Cerebellum | BPPV | Vestibular Neuritis |
| Meniere’s Disease | Cervicogenic Dizziness | Chronic Inflammation |
| Heavy metal toxicity | Food Sensitivities | Food Additives |
| Mould Toxicity |
A highly-skilled (Functional) practitioner can evaluate all of the following:
-
Brain Hemispheres
The brain’s hemispheres can be linked to vertigo, but the connection is complex and not fully explained by hemispheric differences alone. Vertigo, a sensation of spinning or dizziness, often stems from issues in the vestibular system, which includes parts of the inner ear and brain regions like the cerebellum, brainstem, and vestibular cortex. These areas process balance and spatial orientation.
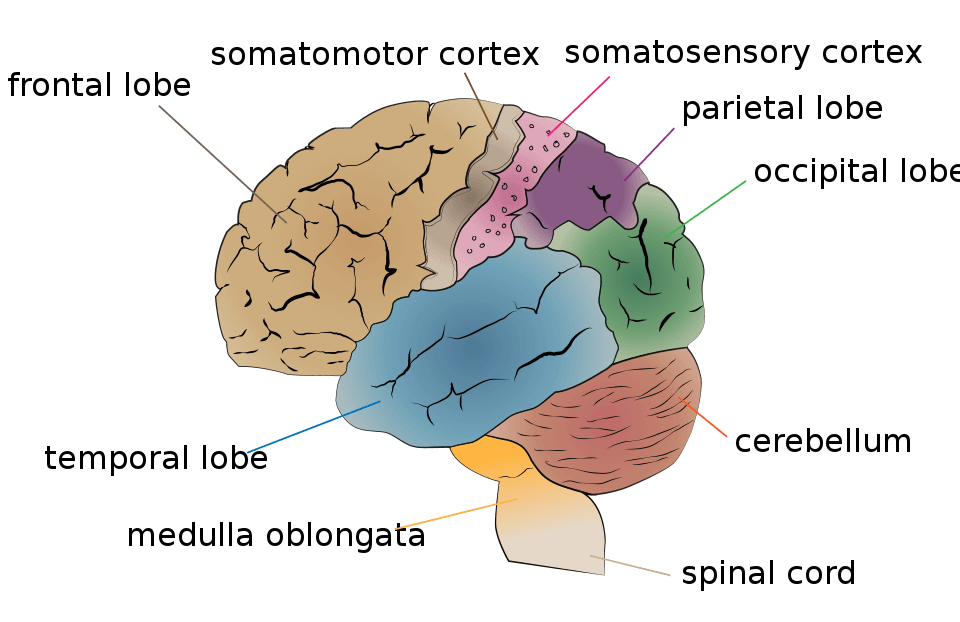
The vestibular cortex, located in the parietal and temporal lobes, is distributed across both hemispheres but shows some lateralization. The right hemisphere is often more dominant in processing spatial orientation and vestibular signals in right-handed individuals, while the left hemisphere may play a stronger role in left-handers. This asymmetry can influence how vestibular dysfunction manifests. For example, lesions or disruptions in the right parietal cortex might cause vertigo or spatial disorientation due to its role in integrating vestibular, visual, and proprioceptive inputs.
There’s no direct evidence that one hemisphere “causes” vertigo, but imbalances in hemispheric processing can contribute.
-
Vagal Nerve
The vagal nerve is linked to vertigo, though the connection is complex and not always direct. The vagal nerve, a key part of the parasympathetic nervous system, influences heart rate, blood pressure, and inner ear function, all of which can contribute to balance and dizziness. Dysfunction or overstimulation of the vagal nerve, such as in cases of vasovagal syncope, can lead to symptoms like dizziness or lightheadedness, which may be mistaken for vertigo. Additionally, the vagus nerve interacts with the vestibular system (responsible for balance) via connections in the brainstem, so issues like inflammation, compression, or autonomic dysregulation could indirectly trigger or worsen vertigo.
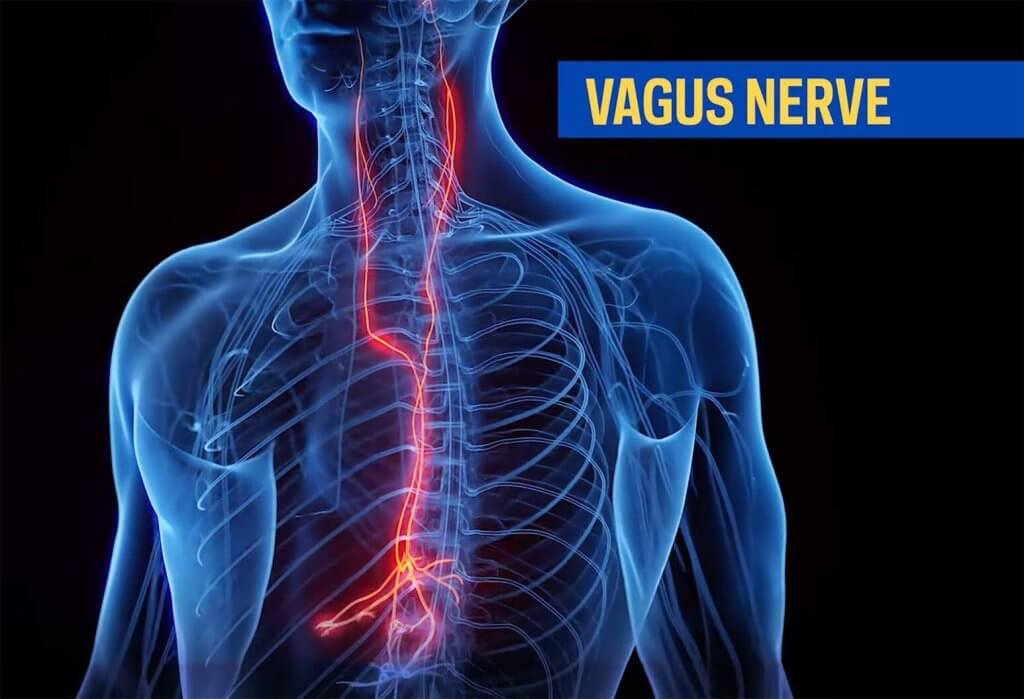
Conditions like vestibular neuritis, migraines, or autonomic disorders (e.g., POTS) can involve vagal nerve dysfunction and are associated with vertigo. For example, vagal nerve irritation might affect blood flow to the inner ear, contributing to balance issues. However, true vertigo (a spinning sensation) is more commonly tied to inner ear disorders (e.g., BPPV, Meniere’s disease) or central nervous system issues than solely vagal nerve problems.
-
Ponto Medullary Reticular Formation
The pontomedullary reticular formation, located in the brainstem, plays a role in coordinating various functions, including balance, posture, and eye movements, which are mediated through its connections with the vestibular system.
The pontomedullary reticular formation is not directly the primary cause of vertigo, but it is involved in processing vestibular information and relaying signals to other parts of the brain, such as the cerebellum and oculomotor nuclei, to maintain balance and coordinate eye movements. Dysfunction in this region—due to lesions, ischemia, or other neurological conditions—can disrupt these pathways, potentially contributing to symptoms like vertigo or related balance disorders.
-
Cerebellum
The cerebellum can be linked to vertigo. The cerebellum, located at the back of the brain, plays a key role in coordinating movement, balance, and spatial orientation.
Dysfunction in the cerebellum, such as from stroke, tumors, inflammation, or neurodegenerative conditions, can disrupt these functions, leading to vertigo. For example, cerebellar disorders can affect the vestibular system’s ability to maintain balance, causing symptoms like vertigo, nausea, and unsteadiness.
-
Benign Paroxysmal Positional Vertigo (BPPV)
The most prevalent form of vertigo, BPPV occurs when tiny calcium carbonate crystals (otoconia) become dislodged and migrate into the semicircular canals of the inner ear. This misplacement interferes with normal fluid movement, triggering intense, brief episodes of vertigo with changes in head position.
-
Vestibular Neuritis or Labyrinthitis
Inflammation of the vestibular nerve (neuritis) or both the nerve and the cochlea (labyrinthitis) can result from viral infections. This causes sudden, severe vertigo that may be accompanied by nausea, imbalance, and hearing changes.
-
Meniere’s Disease
This chronic inner ear disorder involves fluctuating pressure and fluid build-up in the labyrinth. Symptoms include vertigo, tinnitus (ringing in the ears), hearing loss, and a sense of fullness in the ear.
-
Cervicogenic Dizziness
Originating from dysfunction or injury in the cervical spine, especially following whiplash or poor posture, this form of vertigo is related to proprioceptive input rather than inner ear abnormalities.
-
Chronic inflammation
Chronic inflammation may be linked to vertigo in some cases, particularly when inflammation affects the inner ear, nervous system, or related structures. Here’s a concise overview:
Inner Ear Inflammation: Conditions like labyrinthitis or vestibular neuritis, often triggered by infections or inflammatory responses, can cause vertigo. Chronic inflammation in the inner ear may disrupt balance and spatial orientation.
Autoimmune Disorders: Chronic inflammatory conditions, such as rheumatoid arthritis or lupus, can affect the vestibular system, potentially leading to vertigo.
Vascular Inflammation: Chronic inflammation in blood vessels (e.g., vasculitis) may reduce blood flow to the brain or inner ear, contributing to dizziness or vertigo.
Neurological Impact: Chronic inflammation in the brain, as seen in conditions like multiple sclerosis, can affect the vestibular nerve or brain regions responsible for balance.
-
Heavy metals
Heavy metal toxicity can be linked to vertigo. Exposure to toxic metals like lead, mercury, cadmium, and arsenic may damage the nervous system, including the vestibular system, which controls balance. This can lead to symptoms like dizziness, vertigo, and coordination issues. For example:
Lead: Can impair the inner ear and vestibular nerve, causing balance disturbances.
Mercury: Known to affect the central nervous system, potentially leading to vertigo and tremors.
Cadmium and Arsenic: May cause neurotoxicity, contributing to dizziness and spatial disorientation.
Studies suggest chronic exposure, often through contaminated water, food, or occupational hazards, increases the risk. Diagnosis typically involves blood or urine tests to measure metal levels, and treatment may include chelation therapy to remove metals.
-
Food Sensitivities and additives
Food sensitivities may contribute to vertigo in some cases, though the link is not fully understood and varies by individual. Certain foods or additives can trigger symptoms that resemble or exacerbate vertigo, particularly in people with underlying conditions like vestibular migraines or Meniere’s disease.
Here’s a breakdown of the potential connections:
Vestibular Migraines: Food sensitivities, such as to gluten, dairy, or MSG, can trigger migraines, which may include vertigo as a symptom. For example, gluten sensitivity in celiac disease has been associated with neurological symptoms, including dizziness and balance issues, in some studies.
Meniere’s Disease: This inner ear disorder, characterized by vertigo, tinnitus, and hearing loss, can be influenced by dietary factors. High salt intake, caffeine, alcohol, or certain food sensitivities (e.g., to gluten or dairy) may worsen symptoms in some individuals by affecting fluid balance in the inner ear.
Inflammation and Histamine: Food sensitivities can cause systemic inflammation or histamine release, which may affect the vestibular system. For instance, histamine intolerance from foods like aged cheeses, fermented products, or alcohol could lead to dizziness or vertigo in sensitive individuals.
Blood Sugar and Dehydration: Sensitivities to high-sugar or processed foods can cause blood sugar fluctuations or dehydration, which may indirectly contribute to dizziness or vertigo-like sensations.
Allergic Responses: Allergic reactions to foods (e.g., nuts, shellfish) can occasionally cause dizziness or lightheadedness, though true vertigo is less common. These reactions may involve histamine or immune responses affecting blood flow or inner ear function.
-
Mould Toxicity
Mould toxicity can be linked to vertigo. Exposure to certain moulds, particularly those producing mycotoxins, can cause neurological symptoms, including dizziness and vertigo. This happens because mycotoxins may affect the central nervous system, disrupt inner ear function, or cause inflammation that impacts balance. Symptoms often arise in individuals exposed to mould in damp or poorly ventilated environments.
Studies and clinical reports suggest a connection, though direct causation is hard to prove due to individual variability and coexisting factors. For example, a 2017 study in Clinical Reviews in Allergy & Immunology noted that mould exposure can contribute to neurological symptoms, including dizziness, in sensitive individuals.
What Are the Typical Symptoms Associated With Vertigo?
Vertigo may present with a wide array of symptoms, depending on the underlying cause. Common features include:
- Sensation of spinning or tilting
- Nausea and vomiting
- Unsteadiness or imbalance
- Difficulty focusing or blurry vision
- Nystagmus (involuntary eye movements)
- Headaches or migraines
- Tinnitus or hearing loss (in some cases)
These symptoms can be intermittent or continuous and may worsen with head movement or certain positions, particularly in BPPV.
How Can (Functional) Physiotherapy and Integrative Health Help in the Treatment of Vertigo?
| Brain Hemispheres | Vagal Nerve | PMRF |
| Cerebellum | BPPV | Vestibular Neuritis |
| Meniere’s Disease | Cervicogenic Dizziness | Chronic Inflammation |
| Heavy metal toxicity | Food Sensitivities | Food Additives |
| Mould Toxicity |
Physiotherapy is a cornerstone in the management of many vestibular disorders, particularly BPPV, vestibular hypofunction, and cervicogenic dizziness. Our approach at the West Perth clinic is holistic — we not only address the immediate vestibular dysfunction but also the related postural, muscular, and neurological systems that contribute to a patient’s overall sense of balance and orientation.
(Functional) Physiotherapy and Integrative Health aims to establish the Root Cause of your Vertigo and then provide adaptive therapies to overcome the vertigo.
- Retrain the brain to adapt to vestibular imbalance (vestibular rehabilitation)
- Reposition displaced inner ear crystals (in BPPV)
- Restore normal head and neck function (in cervicogenic dizziness)
- Improve strength, coordination, and postural control
- Reduce anxiety associated with vertigo episodes
What Specific (Functional) Physiotherapy and Integrative Health Treatments Are Effective for Vertigo and Why?
The treatment approach is guided by a thorough assessment and depends on the cause of vertigo. Some of the most effective techniques include:
-
Lifestyle Modification
- Improving quality of sleep
- Lowering stress levels
- Avoiding alcohol
- Avoiding coffee (and other food items that often have mycotoxins)
- Cleaning up the diet (whole food diet, organic, pesticide-free, hormone-free, sugar-free)
- Clean water supply (purified drinking water, clean cooking water, filtered water for showering)
- Avoiding chemicals in personal care products.
- Avoiding chemicals in home cleaning products.
- Daily movement with 10,000 steps per day
-
Retrain the brain to adapt to vestibular imbalance.
- Colour therapy
- Aromatherapy
- Vagal nerve exercises
- Eye exercises
- Lymphatic massage
- Breathwork exercises
- Cerebellar exercises
- PMRF exercises
-
Canalith Repositioning Techniques (CRT)
For BPPV, manoeuvres such as the Epley, Semont, or Barbecue Roll (Lempert) are used to guide displaced otoconia back to their proper location in the utricle. These are highly effective, with success rates often exceeding 80% after just a few sessions.
-
Vestibular Rehabilitation Therapy (VRT)
VRT involves a series of customized exercises to promote central compensation by the brain. These include:
- Gaze Stabilization Exercises (e.g., VOR x1 and x2 exercises): Improve the vestibulo-ocular reflex to maintain visual focus during head movements.
- Habituation Exercises: Reduce sensitivity to motion stimuli through repeated exposure.
- Balance and Gait Training: Enhance postural control and reduce fall risk.
-
Cervical Spine Manual Therapy
When vertigo is linked to neck dysfunction, manual therapy techniques — including joint mobilizations, myofascial release, and postural retraining — can alleviate symptoms by restoring normal proprioceptive feedback.
-
Neuromuscular Re-Education
Exercises aimed at retraining muscle activation patterns, particularly in the neck and core, support better alignment and coordination, reducing vertigo episodes.
-
Breathwork and Autonomic Regulation
As part of our holistic philosophy, we incorporate breathing techniques and mindfulness practices to calm the autonomic nervous system, which is often heightened during vertigo episodes, contributing to nausea and anxiety.
-
Where required, advanced forms of testing can be completed
- Blood work
- Mould testing
- Heavy metal testing
- Gut Microbiome Testing
- Food Sensitivity Testing’
- Oral Microbiome Testing
What Can a Patient Expect in the First Few Treatment Sessions?
At our West Perth clinic, the first session begins with a comprehensive assessment.
This includes:
- A detailed medical and symptom history
- A detailed analysis of a 3-day lifestyle diary including review of all meds and supplements
- Balance and gait analysis
- CO2 load tolerance
- Vagal nerve assessment
- Advanced nervous system checks
- Eyesight assessment
- Oxygen saturation
- Blood pressure
- Primitive reflex patterns assessed
- Head-to-toe analysis of all joints, muscles, muscle length, neural gliding, reflexes, power
(toes, feet, ankles, knees, hips, sacrum, lumbar spine, thoracic spine, cervical spine, jaw, shoulders, elbows, wrists, fingers)
- Positional tests such as the Dix-Hallpike manoeuvre
- Oculomotor and vestibulo-ocular reflex testing
Based on the findings, an individualised treatment plan is developed. Early sessions may include:
- Lifestyle modification
- Discussions around current medications
- Discussions around current supplements
- ‘Brain Retraining’ exercises
- Cerebellar exercises
- Vagal nerve exercises
- Breathwork
- Performing CRT manoeuvres (if BPPV is diagnosed)
- Beginning VRT with simple gaze stabilization or habituation exercises
- Education on self-management strategies and triggers to avoid
- Manual therapy to restore balance to the body
- Guidance on safety and fall prevention during flare-ups
As treatment progresses, the program becomes more challenging, integrating dynamic movements, head turns, and multitasking activities to mimic real-life scenarios and build resilience.
Final Thoughts
Vertigo can be a complex and distressing experience, but with the right assessment and targeted (Functional) physiotherapy and Integrative Health therapy, many individuals experience significant — often complete — relief from their symptoms. At our West Perth clinic, we take a holistic, patient-centred approach, integrating traditional vestibular techniques with broader strategies to support the nervous system, posture, and emotional wellbeing.
If you or a loved one is dealing with vertigo, don’t let it control your life. Reach out to our expert team for a tailored assessment and evidence-based care that goes beyond symptom management — toward lasting recovery and renewed confidence in movement.
CONTACT US
